Even though implementation of artificial intelligence (AI) in the field of dermatology is not infallible, it could result in greater diagnostic capabilities and optimized patient care outcomes, says GlobalData, a leading data and analytics company. AI in dermatology not only has potential in alerting people when they may need to see a doctor (usually through the use of a smart device), it can also be used to create an educational resource for medical students, as well as a confidence boost to physicians making a differential diagnosis. One notable application has been the training of a convolutional neural network (CNN) to more accurately diagnose melanoma and less often misdiagnose benign moles. This method has been shown to demonstrate greater sensitivity and specificity than 58 international dermatologists, according to the European Society for Medical Oncology (ESMO) in May 2018. Antoine Grey, Pharma Analyst at GlobalData, comments: “A CNN is trained to compare a new image to the most visually similar images from a pre-established library of images that capture the same pathology. Through machine learning, the CNN can teach itself from what it has learned to improve performance.”
In a study published by ESMO, it was revealed that when calibrated to identify benign moles to the same extent as the 58 dermatologists, the CNN correctly identified 95% of melanomas from a sample of 100 images, whereas the dermatologists identified 86.6% of melanomas.
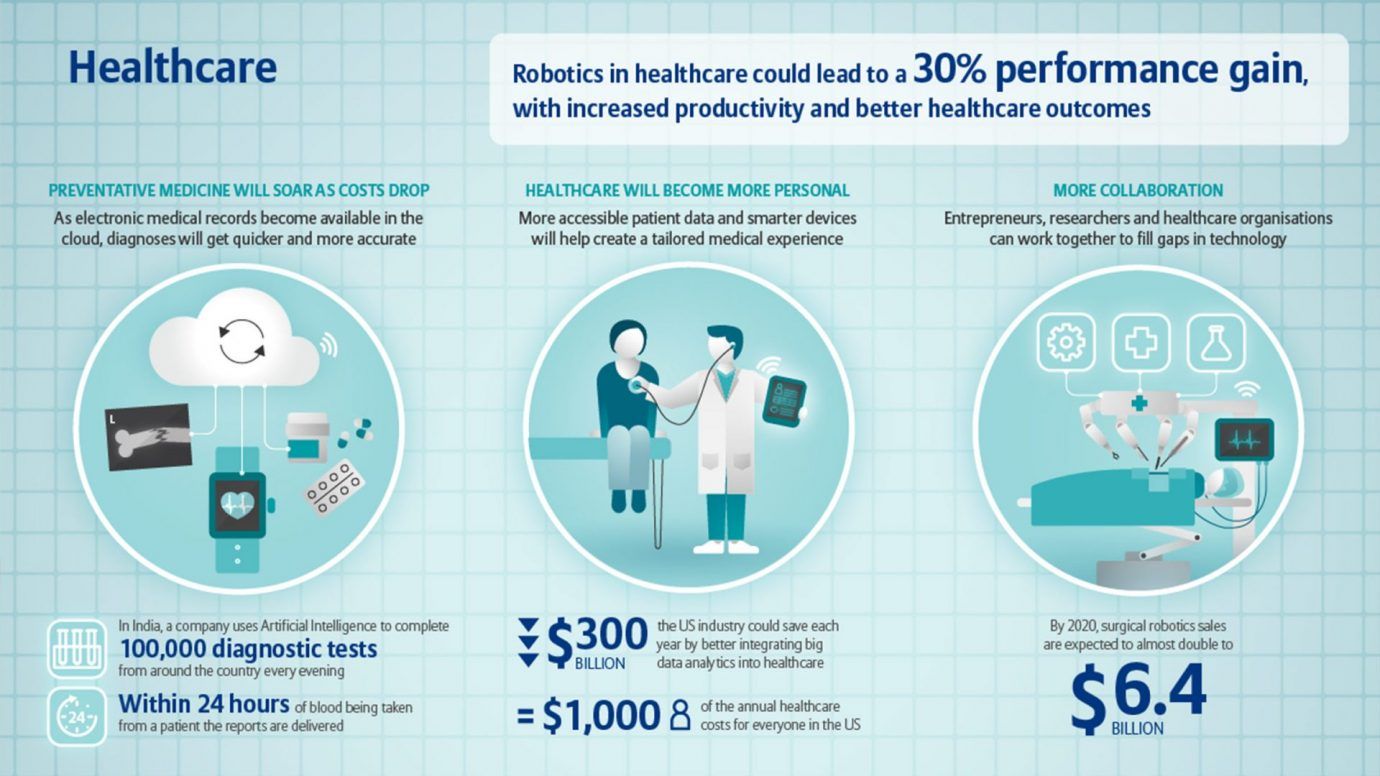 Healthcare innovations and AI. Source: Allianz
Healthcare innovations and AI. Source: Allianz
Another example of integrating AI in dermatology is the appearance of tele-dermatology companies such as First Derm. These companies produce applications, which help patients in deciding whether they need to see a doctor in person or not. Grey adds: “As a result, the patient can have peace of mind and dermatologists are not inundated with unnecessary patient visits that could easily be solved by over-the-counter medication.”
However, access to medical data sets needed to train AI can be difficult to attain at the scale necessary for training due to the need for patient consent and the potential requirement of approval from relevant ethics boards. Moreover, the clinical data sets used for training are clinical images taken with a dermascope under controlled conditions; comparison of clinical data sets to images taken with a mobile phone in poor lighting conditions may lead to misdiagnoses. Another issue for AI may be the inability to distinguish between visually similar conditions with different causes, such as rashes caused by infection compared to rashes caused by a drug reaction. Lastly, there is the potential for racial disparity in machine learning for skin cancer screenings. This was seen in the study published by ESMO, where there were far fewer images of patients that were not Caucasian, raising concerns that the mortality rate for African Americans developing melanoma will remain higher than in Caucasians even with the advent of AI in dermatology, despite Caucasians having a much higher risk of developing melanoma. Grey concludes: “The implementation of AI in dermatology does present several issues that need to be addressed. However, it has potential to provide significant benefit to both patients and dermatologists alike.”